5 Myths About Formula-Feeding, Debunked
When it comes to feeding baby, everyone has an opinion. And while some of that well-meaning advice may be hard to ignore, a lot of it isn’t based on fact. That’s why we reached out to leading experts to help break down some common myths and misconceptions when it comes to baby formula. Whether you choose to exclusively breastfeed, formula-feed or do a combo of the two, the best choice is always to do what’s going to meet your and your child’s unique needs.
Bonding with baby comes down to two important factors: skin-to-skin contact and facial recognition, not just baby’s connection to your breast. So don’t worry that a bond won’t form simply because you’re bottle-feeding. Need some tips for establishing that cherished attachment while using a bottle? “Practice skin-to-skin contact, look directly into baby’s eyes and talk or sing to baby while you feed them a bottle,” suggests Nina Pegram, PNP, IBCLC, a pediatric nurse practitioner and lactation consultant at SimpliFed. “Whether it includes a bottle or a breast, never fear, bonding will occur.”
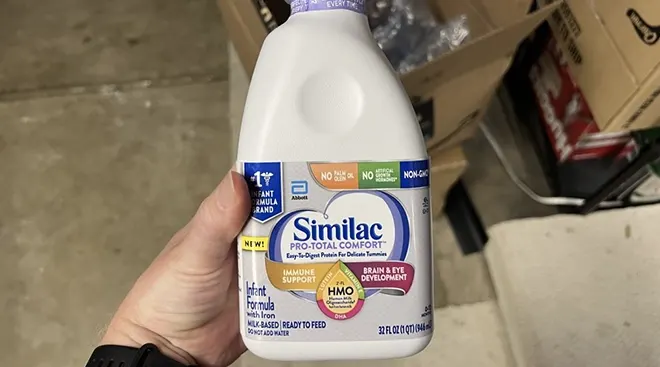
It’s true that when mass-market baby formula was first introduced, there were developmental differences between breastfed and formula-fed infants. But the good news is today’s formulas have come a long way. By gaining a better understanding of human breast milk composition, formula manufacturers have been able to more accurately determine the nutrient types and ratios that contribute to optimal growth in babies.
Infant formulas now include critical brain-boosting ingredients like DHA and ARA, two of the things that used to give breastfed babies an edge over their formula-fed counterparts. And while you can still find studies that assert that breastfed babies maintain an advantage, you can find others that state the relationship is inconclusive. In one telling study published in the British Medical Journal, researchers looked at IQ levels of siblings with the same mother where one breastfed and the other did not, and found that there were no “cognitive advantages of breastfeeding.”
“A child’s intelligence level is influenced by a variety of factors, including many things that are largely outside of parental control, such as genetics,” says Crystal Karges, RDN, IBCLC, a maternal child health specialist at Crystal Karges Nutrition. “There is no scientific evidence to suggest that formula-fed babies won’t be as smart as breastfed babies.”
“This one is a real kicker! Lots of infants need pacifiers or artificial nipples for various health related issues and have no problems switching between the two,” Pegram says.
Any issues with baby fussing or refusing the breast or bottle may just come down to baby’s nipple preference, rather than nipple confusion. You can always experiment with different shaped nipples to see what works best, but for starters, try a wide-mouth, slow-flow nipple to help mimic how they feed at the breast. You’ll also want to adjust baby’s position to make sure they can pace their feed. “If milk is dripping out of the infant’s mouth, it’s flowing too quickly, so sit them up a bit more,” Pegram says. “If baby seems to ‘prefer’ the bottle, then try more at-the-breast time. If they start ‘chomping’ a bit or causing pain when they go back to the breast from the bottle, then ease up on the frequency of bottle feeds.”
While this is far from a universal truth, it’s not entirely false. That’s because breastfeeding is a supply-and-demand process, and your body makes more milk depending on how often you breastfeed (or pump). “So in theory, if you’re not draining your breasts when your baby takes the formula supplement, this can be true. Your body will think that the baby got all of the milk that it needs” and may scale back on production, Pegram explains. If your goal is to breastfeed exclusively for any amount of time (and the AAP recommends it exclusively for baby’s first six months), you’ll need to keep supplementing with formula to a minimum, and be sure to pump anytime you supplement.
Still, giving baby small amounts of formula doesn’t mean your milk will dry up. “It can actually be the complete opposite in some cases,” says Kathy Murphy, IBCLC, another lactation consultant at SimpliFed. “By supplementing, we can often give the baby the energy and calories needed to become a more efficient and vigorous feeder at the breast, especially if they’ve been struggling with calorie intake and weight gains.” In fact, a recent study found supplementing with a limited amount of formula for babies with early weight loss can actually help with breastfeeding outcomes when baby gets older.
While formula isn’t an exact replica of a mother’s milk, there’s no need to worry if you end up formula-feeding when baby arrives—today’s formulas are a top-notch alternative to breast milk. According to Karges, ”infant formula is a complete and suitable nutrition source for babies. It’s intended as an effective substitute to breast milk and is formulated to mimic the nutritional composition of breast milk.” To make sure of this, the manufacturing process is highly regulated, and infant formulas have to include proper amounts of water, carbohydrates, protein, fat, vitamins and minerals (per established guidelines) to meet a baby’s nutritional needs. As long as baby isn’t overly fussy, excessively gassy or spitting up frequently, and is growing according to your pediatrician’s recommendations, it’s a good sign your child is getting enough nutrition—regardless of whether you’re breastfeeding or formula-feeding.
About the experts:
Nina Pegram, RN, PNP, IBCLC, is a pediatric nurse practitioner with Northeast Pediatrics in Ithaca, New York, and a lactation consultant at SimpliFed. Before working as a pediatric nurse practitioner, she served as a NICU nurse. She received her Master’s degree in nursing from Rutgers University in New Jersey.
Crystal Karges, RDN, IBCLC, is a maternal child health specialist and registered dietitian nutritionist at Crystal Karges Nutrition. She earned her Master’s degree in nutritional sciences from the University of Saint Joseph in West Hartford, Connecticut and completed a lactation consultant certification program at the University of California, San Diego.
Kathy Murphy, PA-C, IBCLC, is a pediatric physician assistant and a lactation consultant at SimpliFed. She completed her physician assistant degree at LeMoyne College in Syracuse, New York.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.