Postpartum Timeline: Here’s How Soon After Birth You Can Do Things
You’ve been anxiously awaiting baby’s arrival—but let’s be honest, you’ve also been craving a salmon roll, a glass of sauvignon blanc and your normal workout routine. The good news? “Restrictions in pregnancy are almost entirely related to preterm birth risk, so virtually all of these go away after delivery!” says Margaret Dow, MD, ob-gyn and chair of the birth center at Olmsted Medical Center in Rochester, Minnesota. Plus, right when your six-week postpartum checkup rolls around, you can generally do most things you’re told to avoid immediately after childbirth. Wondering what exactly you’ll be able to do after birth and when? Here’s the lowdown, straight from the experts.
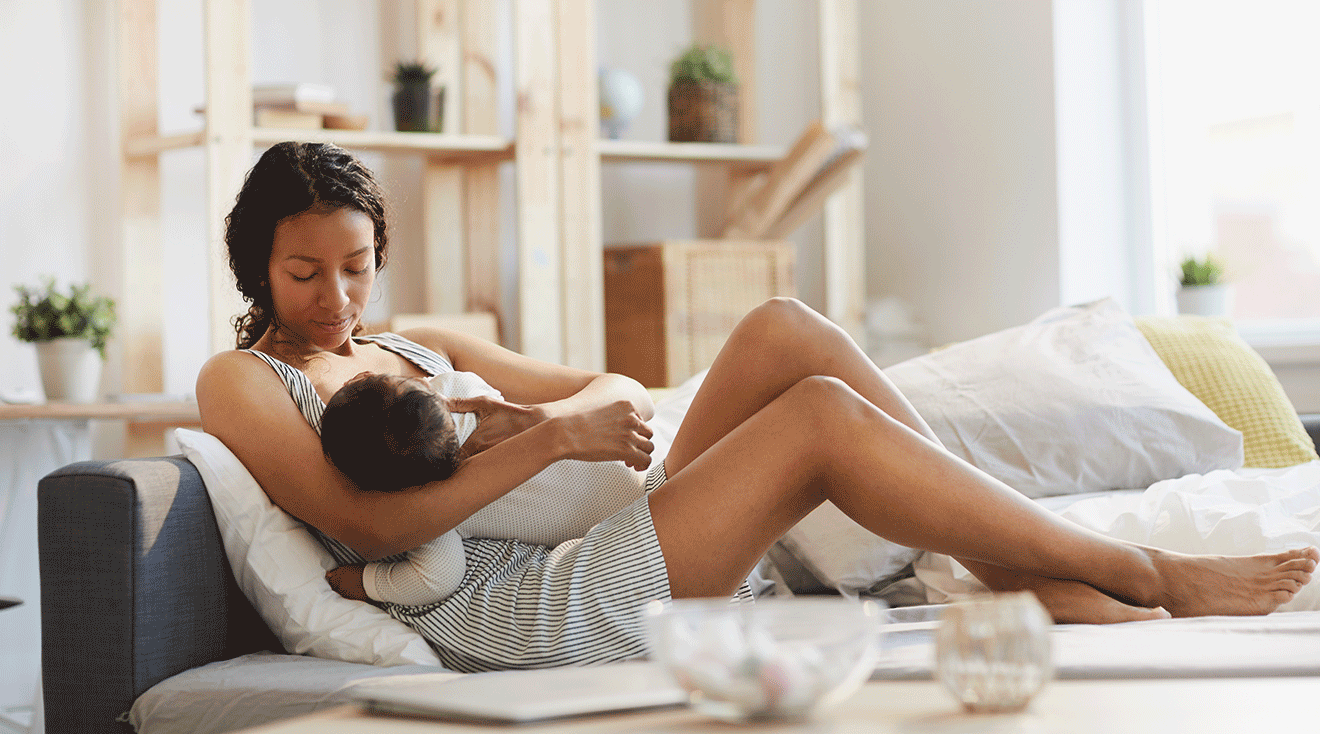
Providers generally make every effort to foster skin-to-skin contact right away after a vaginal birth or C-section, says Danielle Mari Panelli, MD, an ob-gyn and clinical instructor in maternal-fetal medicine at Stanford Medicine. “We generally encourage skin-to-skin contact with baby on Mom’s chest as soon as possible after birth as long as it’s safe, even in the operating room,” she adds. After a C-section, you’ll typically be moved from the operating room to a recovery room, where you can enjoy skin-to-skin more comfortably.
Your team can do many post-birth newborn procedures like checking baby’s vital signs, giving the vitamin K injection and applying eye ointment while baby’s with Mom, so there’s no need to interrupt those newborn snuggles, says Janna Mudd, MD, an ob-gyn with Mercy Medical Center in Baltimore, Maryland. “Immediate skin-to-skin contact helps to promote bonding and breastfeeding, and can even help your baby transition to life outside the womb,” she says.
If there are any complications after your delivery, you might not be able to do skin-to-skin right away, notes Sherry Ross, MD, an ob-gyn and women’s sexual health expert, and the author of She-ology: The Definitive Guide to Women’s Intimate Health. Period. and She-ology, the She-quel: Let’s Continue the Conversation. In these cases, baby may need to be closely monitored by the neonatal team to ensure they’re thriving after delivery, she explains.
Panelli says that how long you stay after birth depends on the hospital and your personal birth experience, including whether there were complications. That said, in general, doctors aim for Mom and baby to go home one to two days after a vaginal birth and three to four days after a C-section.
While some moms want to get out of the hospital ASAP, others prefer a prolonged stay—provided insurance covers it, of course. “Because of how late we originally checked in, they let us stay an extra night, which made for a grand total of almost five nights,” says Natalie G., senior editor at The Bump. “Then I had an intense post-epidural headache on the last day, so they hooked me up to an IV and let us stay another few extra hours. I didn’t want to go home because I felt so well taken care of.”
As soon as you want. Itching for a drink? The good news is you can have one a couple hours after birth, if you really wanted to. “When my first was born, our hospital actually gave us a bottle of Champagne—along with a surf-and-turf lobster and steak dinner,” recalls Lauren B., mom of three and associate content director at The Bump. Of course, for breastfeeding moms, “the timing of the drink is important,” notes Deedra Franke, RN, BSN, IBCLC, a lactation consultant at Mercy Medical Center in Baltimore, Maryland. To be safe, the best time to indulge is right after feeding baby. To avoid passing any alcohol to your little one through your breast milk, “you should wait two to three hours before nursing” after having a single drink, Franke says.
After all that time in the hospital, you might be wondering, “When can I take a bath after giving birth?” Panelli says that after a vaginal birth, providers typically recommend avoiding baths, pools and hot tubs for at least six weeks or until you’re seen for a follow-up visit. However, early on, you’ll likely be encouraged to take a sitz bath—a shallow bath designed to help with perineal healing.
After a C-section, providers often place Steri-Strips, aka thin adhesive bandages, over your incision with another dressing on top. “The outer dressing is typically removed one to two days after birth, and if the incision looks good your doctor will let you know if you can shower,” Panelli says. As far as post-C-section baths and hot tubs, you should wait at least two weeks after giving birth, according to the University of Washington Medical Center. Some providers recommend waiting longer. “Keep in mind that everyone is unique,” says Christine Greves, MD, FACOG, an ob-gyn at the Winnie Palmer Hospital for Women & Babies in Orlando. “If you had a C-section, then you don’t want to weaken those sutures [aka stitches], so we recommend waiting six weeks to allow the healing.” Be sure to check in with your provider about the right timeline for you—they may give you the all-clear sooner, or advise you to wait until your incision has done more healing.
You can often eat—sushi or otherwise—as soon as you want after delivery, although if you had a C-section, your provider will generally tell you to hold off for a couple of hours. “I was advised not to eat solid food for several hours after C-section, but I also didn’t want to,” says Natalie. “I was super-nauseous and just wanted ginger ale. But when I finally had that first meal, it tasted amazing.”
Once you’re able to tolerate eating, there’s no reason not to order some sushi rolls. “You can order some rolls immediately after delivery if you’ve been wanting to eat raw fish,” says Ross. Consuming raw fish is a-okay while you’re breastfeeding, but nursing moms should be careful to avoid eating fish that’s high in mercury, adds Franke. (Salmon, shrimp and whitefish are good low-mercury choices.)
Within hours. Really craving a cup of java? You can probably have one with your post-delivery meal. If you’re drinking coffee while breastfeeding, “the amount of caffeine that gets into breast milk is small,” Dow says, although she notes that some babies seem to show “a little jitteriness” if they get a taste of it. If you’re worried, time your coffee break so it’s right after you nurse rather than right before.
Within one to six weeks. “Mothers who have vaginal deliveries can generally return to exercise sooner than those who have had C-sections,” says Mudd, “but both can do light exercise, such as walking, whenever they feel ready.” We’re talking light here—not strenuous exercises or high-impact aerobics. But walking and Kegel exercises are great ways to ease back into fitness. Moreover, movement can offer some great benefits: Activity can promote better sleep, lower the risk of blood clots and boost your physical health and general well-being, Dow says. As long as everything is healing well, your doctor will likely clear you for all types of exercise at your six-week postpartum appointment.
Many sources say you’ll need to wait until your postpartum bleeding has stopped before you go swimming. This generally happens around six weeks after birth.
You can generally get behind the wheel within one to six weeks. Women who are taking opioid pain medicines definitely shouldn’t drive, but other than that, it really depends on how your individual recovery is going. Especially if you had a C-section, Dow suggests trying this first: Sit in the car and practice moving your foot from the accelerator to the brake and turning to look over your shoulders several times. See if you can do that easily and without pain. Some women are able to do this several days after surgery, and for some it can be a few weeks. Women who had a vaginal delivery but experienced an extensive tear or an episiotomy may also need to keep away from the wheel for a little while, Dow adds.
Doctors will tell you “nothing in the vagina for six weeks,” which translates to no tampons and no sex during that time. “A woman’s body is still healing regardless of the mode of delivery for at least six weeks,” Ross explains. That means you should wait until your doctor gives you the green light at the six-week postpartum appointment before having sex again. If you haven’t healed well, your doctor may ask you to hold off longer. “The first time you have sex, recognize that the vagina may be less lubricated than normal… Especially if [you’re] breastfeeding. Also, it can be tender,” notes Greves.
Of course, when you’re medically cleared for sex and when you’re emotionally ready to have sex are two different things. Between the physical and hormonal changes a woman goes through during pregnancy and after childbirth, plus breastfeeding and the challenges of having a newborn, a lot of couples find that they’re not ready to have sex again right away, and that’s okay. Go at your own pace. “It’s not unusual to have a decline in libido related to dropping hormones, fatigue from the demands of caring for a baby or houseguests such as in-laws coming to help after delivery,” says Cynthia DeTata, MD, an ob-gyn and clinical assistant professor in maternal-fetal medicine at Stanford Medicine. “This is all normal and will change over time.”
You can get a postpartum massage as soon as you’re comfortable, says the American Pregnancy Association (APA), although many healthcare providers generally recommend waiting until four to six weeks after birth. If any part of your body is uncomfortable, your massage therapist will be sure to reposition you. “Many new parents find it physically uncomfortable to lay on their stomach or chest if they’re lactating, though some are able to get modified massages through providers who are familiar with pre- and postnatal body changes,” notes Panelli. If you have any postpartum complications or have any other questions, make sure to consult with your medical provider first.
When you’re getting ready to resume sexual activity, it’s important to start some form of birth control if you’re not looking to conceive. Many people are “cleared” to have sex after six weeks, but keep in mind that ovulation can start as soon as three weeks postpartum. Don’t rely on breastfeeding as a form of contraception, though. “You might not have your period when you’re breastfeeding, but it’s not a good form of birth control,” cautions Allison Boester, MD, assistant professor of clinical obstetrics and gynecology at Weill Cornell Medical Center in New York City. “You can still ovulate and get pregnant.” She generally suggests the pill, condoms or an IUD for new moms. (Opt for a progestin-only pill, which is less likely to affect your milk supply than combination pills.)
Looking for a cheat sheet on what you can do after birth and when? See below.
Immediately after birth
Right after giving birth, you can typically hold baby and breastfeed. If you had a vaginal birth, you can typically eat and drink right away, though you might have to wait a couple of hours after a C-section.
Within 24 hours
You can typically shower within 24 hours after birth. After a vaginal birth, you might also be encouraged to take a sitz bath to help with perineal healing.
Within 48 hours
Within 48 hours postpartum, you can generally go home if you had an uncomplicated vaginal birth. If you had a C-section, you’ll typically wait three to four days.
Two weeks after birth
At this stage, many people are able to take a bath, drive and perform light exercise. Just make sure to clear it with your provider first.
Four weeks after birth
Between four and six weeks after birth, it’s typically safe to get a massage. (And, let’s be honest—you’ll need some pampering after those long nights with baby!) Be sure to talk to your healthcare provider about your individual situation.
Six weeks after birth
During your six-week postpartum appointment, your doctor is likely to clear you for a variety of activities, if they haven’t already. They might tell you that you can have sex (whether or not you want to is a completely different story), exercise—including swim, take a bath, go in a hot tub and drive a car. If you don’t feel ready for a particular activity yet, be sure to go at your own pace.
It might feel confusing to navigate all the after-birth restrictions. But if you stick to this timeline—and ask your provider if you’re unsure of anything—your recovery is more likely to go smoothly.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Allison Boester, MD, FACOG, is an ob-gyn and assistant professor of clinical obstetrics and gynecology at Weill Cornell Medical Center in New York City, where she has been on the faculty since 2005. Boester received her medical degree at the University of Maryland School Of Medicine.
Cynthia DeTata, MD, is an ob-gyn at Stanford Medicine Children’s Health and clinical assistant professor in maternal-fetal Medicine at Stanford Medicine. She earned her medical degree from the University of Southern California Keck School of Medicine.
Margaret Dow, MD, is an ob-gyn and the chair of the birth center at Olmsted Medical Center in Rochester, Minnesota. She has a particular interest in exercise, sleep, nutrition and pregnancy. She earned her medical degree from University of Nevada School of Medicine.
Deedra Franke, RN, BSN, IBCLC, is a lactation specialist at Mercy Medical Center in Baltimore, Maryland, where she has worked since 2010. Franke has served as a certified lactation consultant since 1989 and earned her nursing degree from the University of Maryland School of Nursing in Baltimore in 1981.
Christine Greves, MD, FACOG, is an ob-gyn at the Winnie Palmer Hospital for Women & Babies in Orlando. She received her medical degree from the University of South Florida College of Medicine.
Janna Mudd, MD, is an ob-gyn with Hoffman and Associates, an all-female ob-gyn doctor group affiliated with Mercy Medical Center in Baltimore, Maryland. She earned her medical degree at Drexel University College of Medicine, Philadelphia. She is a junior fellow of the American College of Obstetricians and Gynecologists and a member of the American Medical Association Society for Obstetric Anesthesia and Perinatology.
Danielle Mari Panelli, MD, is an ob-gyn at Stanford Medicine Children’s Health and a clinical instructor in maternal-fetal medicine at Stanford Medicine. She earned her medical degree from the University of California San Diego School of Medicine.
Sherry Ross, MD, is an ob-gyn and women’s sexual health expert. She’s the author of She-ology: The Definitive Guide to Women’s Intimate Health. Period. and She-ology, the She-quel: Let's Continue the Conversation. She received her medical degree from New York Medical College.
Tommy’s, What Happens After a C-Section?, July 2021
University of Washington Medical Center, After Your Cesarean Birth, September 2016
Lee Health, Preparing for Your Cesarean Section
Public Health Scotland, Getting Active After the Birth, December 2023
American Pregnancy Association, Postpartum Massage
Chicago Department of Public Health, Caring for Yourself After Delivery
Learn how we ensure the accuracy of our content through our editorial and medical review process.
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.