What Your HCG Levels Might Mean During Pregnancy
Pregnancy comes with a slew of new terms and lingo to learn. And given that you probably don’t have a background in obstetrics, it’s understandable to have questions. One medical acronym that may come up early on in your pregnancy is hCG. It stands for human chorionic gonadotropin, and it can give you—and your doctor or midwife—some insight into how your pregnancy is progressing. But what is hCG exactly, and what can your hCG levels by week mean? Here’s what you need to know.
At a basic level, human chorionic gonadotropin is a hormone that supports your pregnancy. “It’s very important in establishing and maintaining the pregnancy through helping with the placenta and development of the early embryo,” explains Christine Greves, MD, an ob-gyn at the Winnie Palmer Hospital for Women & Babies in Orlando, Florida. And, yes, it may also be what’s driving your morning sickness and causing a few other early pregnancy symptoms, according to the Mayo Clinic.
Initially, hCG is secreted to help maintain the corpus luteum—a collection of cells that make the uterus a healthy place for pregnancy—adds Julie Lamppa, APRN, a certified nurse-midwife at the Mayo Clinic. Eventually, your placenta—the organ that provides oxygen and nutrients to your growing baby—will take over progesterone production and hCG levels will dip (more on that below).
The body starts producing the hCG hormone about 10 to 11 days after you conceive, says Kjersti Aagaard, MD, PhD, a professor of obstetrics and gynecology at Baylor College of Medicine in Houston, Texas. “HCG’s claim to fame is that it’s the hormone that’s detected on both urine and blood pregnancy tests.” When measuring hCG levels, your doctor will refer to something called beta hCG levels. In a nutshell, beta hCG levels note the exact amount of the pregnancy hormone in a person’s blood, while the qualitative hCG simply measures whether or not the pregnancy hormone is present in the blood, explains Sherry Ross, MD, an ob-gyn and women’s sexual health expert.
So when is hCG detectable during pregnancy? Urine pregnancy tests can detect hCG levels when they reach 20 to 50 milli-international units/mL, while blood tests are positive at 5 milli-international units/mL, Lamppa says. That typically translates to getting a positive urine pregnancy test around the time your period is due. “It usually takes about two weeks after conception for hCG to be high enough in your urine to be detected,” Greves notes. For a blood test, the hCG hormone is usually detectable 10 days after [conception], Ross adds.
If you’re anxiously waiting for a positive pregnancy test result, try taking your test early in the day. In general, “first morning urine is recommended because it’s when the urine is the most concentrated, and therefore lower levels can be detected more quickly,” says Melissa Goist, MD, an ob-gyn from the Ohio State University Wexner Medical Center. If you get a negative, you can wait and try again; in a healthy pregnancy, hCG levels tend to double every 48 to 72 hours in the early days and weeks of pregnancy, according to Ross and the American Pregnancy Association
“Once a pregnancy test turns positive, most commonly there’s no reason to assess beta hCG level,” Aagaard says. “The overwhelming majority of pregnancies will never have a reason to check a beta hCG level.” There are a few specific scenarios where your beta hCG levels might need to be checked, though. “These include situations where we’re trying to decipher whether a very early pregnancy is developing normally in the uterus, or if there’s a risk of an inevitable miscarriage,” Aagaard says. “To decipher this, we have to measure the beta hCG twice two to three days apart.” Basically, the first level gives your doctor a baseline, the second helps them determine if hCG is rising as expected or declining prematurely. The latter could indicate a potential pregnancy loss.
Lamppa adds that if there’s the suspicion of an ectopic pregnancy (when implantation occurs outside of the uterus), measuring hCG level can be revealing. Of course, a hCG blood test alone isn’t diagnostic, and an ultrasound is necessary to confirm, notes the Cleveland Clinic.
Another scenario that might warrant more thorough testing of your hCG levels in pregnancy? If you’ve conceived through in-vitro fertilization (IVF), your doctor might monitor your levels more closely, says Lamppa.
It’s important to know that levels of hCG typically only increase until a certain point in your pregnancy. According to experts, hCG will peak sometime between weeks 8 and 12, before starting to decrease. But why do hCG levels begin to fall during this time? It’s because your placenta has developed enough to take over and can start supplying progesterone to your pregnancy to help it progress, Lamppa explains.
Until then, while there’s a range of hCG levels that doctors expect to see during certain parts of your pregnancy, everyone’s numbers—and normal hCG levels by week—are a bit different. This is due to the number of trophoblastic cells, which are cells that help your developing embryo attach to your uterus, protect your embryo and form part of your placenta, Goist says. The exact number is “different with each pregnancy,” she adds.
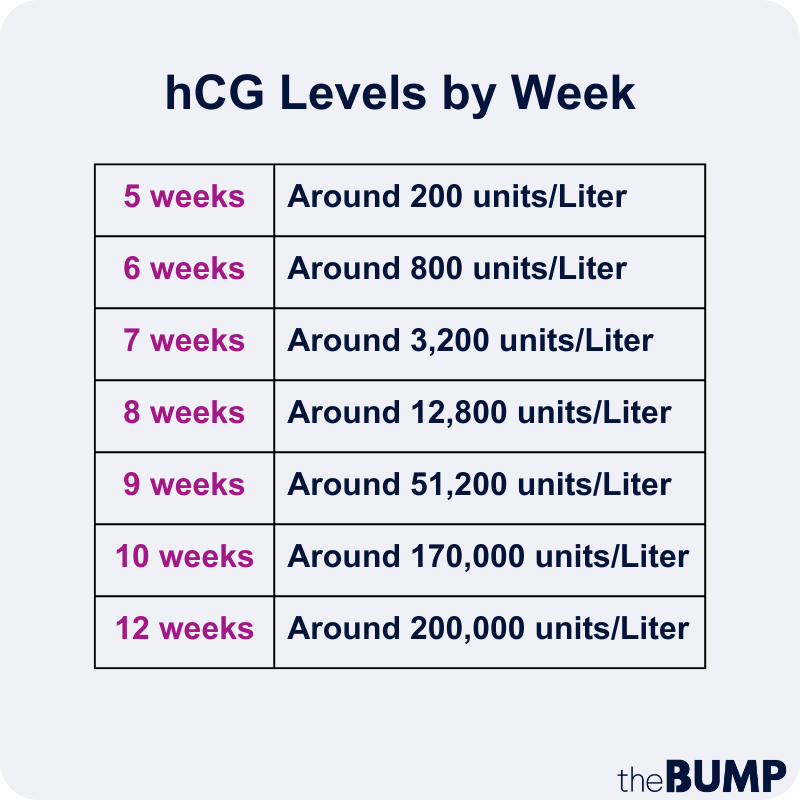
HCG levels chart
The hCG levels chart shows what hCG levels by week can look like during the first trimester. Of course, take this with a grain of salt. “Clinically speaking, as providers, we don’t even look at these [charts], nor depend upon them,” Lamppa says. HCG levels in pregnancy are just too subjective.
The hCG hormone may be to blame for your morning sickness and other early pregnancy symptoms. Ross notes some symptoms of rising hCG levels include:
- Nausea and vomiting
- Fatigue
- Breast tenderness
- Dizziness
- Food cravings
- Intestinal changes
- Increased urinary frequency
According to Greves, if you’re pregnant with twins or multiples, your hCG levels may be higher than if you were having a singleton. (But a high hCG level doesn’t automatically mean you’re expecting more than one baby—again, levels of hCG can vary by person and pregnancy.) In fact, Lamppa says high hCG levels can be normal with a singleton pregnancy or a multifetal one. They can also happen with an ectopic or molar pregnancy, which is a pregnancy that’s not viable. In certain cases, high hCG levels can also suggest certain types of cancers, Ross notes.
It’s true that early on, declining hCG levels could mean a pregnancy isn’t developing properly or suggest an ectopic pregnancy or loss. On the flip side, lower levels could also suggest “an early healthy pregnancy,” Ross notes. It could be “[normal] based on how far the pregnancy has advanced,” Lamppa adds.
Suffice it to say, don’t panic if you learn your hCG levels are on the low side—it might not mean anything, Aagaard says. She adds that, for this reason, doctors and midwives don’t typically check beta hCG levels unless it’s deemed necessary. “It most commonly leads to more testing and increased anxiety,” she adds.
It’s natural to want to do everything you can do to maintain a healthy pregnancy, and it’s scary knowing that declining hCG in early pregnancy might mean an impending miscarriage. Unfortunately, since the hormone is produced and controlled by the body, there’s really nothing you can do to raise (or lower) your hCG levels during pregnancy, Ross says. This is one of those things you simply can’t control.
Frequently Asked Questions
What hCG level indicates pregnancy?
According to Ross, “HCG levels above 25 milli-international units/mL indicate pregnancy.” Monitoring these levels along with performing an ultrasound can help confirm a healthy pregnancy.
What hCG level indicates miscarriage?
Experts don’t point to a certain hCG level to indicate miscarriage. Instead, Ross notes that hCG levels that are low—or even rising irregularly—may suggest a possible miscarriage, especially when accompanied by other symptoms like vaginal bleeding and cramping.
Determining whether your hCG levels are normal can be confusing, to say the least, especially since there isn’t a medically accepted standard. Don’t hesitate to bring up any questions with your provider, especially if they’re keeping tabs on your levels of hCG. Otherwise, experts say it’s not something you need to think twice about.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Kjersti Aagaard, MD, PhD, is a professor of obstetrics and gynecology at Baylor College of Medicine. She received her medical degree from the University of Minnesota Medical School in Minneapolis.
Christine Greves, MD, is an ob-gyn at the Winnie Palmer Hospital for Women & Babies in Orlando, Florida. She received her medical degree from the University of South Florida College of Medicine.
Melissa Goist, MD, is an ob-gyn from the Ohio State University Wexner Medical Center. She received her medical degree from the Medical College of Ohio at Toledo.
Julie Lamppa, APRN, is a certified nurse-midwife at the Mayo Clinic and author of Obstetricks.
Sherry Ross, MD, is an ob-gyn, women’s sexual health expert and author of She-ology: The Definitive Guide to Women’s Intimate Health. Period. and She-ology, The She-quel: Let’s Continue the Conversation. She earned her medical degree from New York Medical College.
Cleveland Clinic, Corpus Luteum, January 2024
American Pregnancy Association, What are HCG Levels?
Cleveland Clinic, Ectopic Pregnancy, January 2023
Mayo Clinic, Is nausea during pregnancy a good sign?, October 2021
Learn how we ensure the accuracy of our content through our editorial and medical review process.
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.